Extra Information
Warning
The diseases described on the following pages contain images and film material taken during operations. Decide for yourself if you want to see these images. Please also note our imprint and the legal information. The Baermed practice assumes no liability. Do you really want to see the page!
HERNIA
Topics
1. Soft tissue fracture
Symptoms and diagnosis of hernias
Hernias (soft tissue hernias) are congenital or acquired gaps in soft tissue through which the contents of the abdominal cavity, including the peritoneum, can bulge through the actual abdominal wall into the subcutaneous tissue.

What is a soft tissue hernia and where does it occur?
A soft tissue hernia is a protrusion in the area of the abdominal wall. It forms in regions that are anatomical weak points in the abdominal wall. Therefore, there are many different types of soft tissue hernias, for example, in the groin, at the umbilicus, at the edge of the straight abdominal muscles or after abdominal surgery in the area of an abdominal wall scar. Read more >
The protrusion is caused by the leakage of abdominal contents, which are enclosed by a hernia sac and escape from the abdominal cavity in front of the abdominal wall through a weak area in the abdominal muscles, the hernia gap. In males, the most common exit site is found in the groin area, where the vas deferens and the vessels necessary to supply the testis pass through the abdominal wall into the inguinal canal in the inner inguinal ring. In women, the round uterine ligament runs from the abdominal cavity into the inguinal canal at the corresponding point and extends from the uterus to the symphysis (pubic bone); soft tissue hernias can also occur in its course. A hernia sac (Fig.1) may contain parts of abdominal organs such as cusps of the large mesh, colon or small intestine. Without treatment, these fractures can assume grotesque sizes.
The most common soft tissue hernias are inguinal hernias, which occur predominantly in men. These will be described in more detail below.

The inguinal hernia as a particularly common soft tissue hernia
The inguinal hernia is called “inguinal hernia” in medical jargon (lat. inguina = the groin). Like any soft tissue hernia, it consists of a prominence that may be visible outside the abdominal wall, a hernia sac, the hernia sac contents, and a hernia gap. Two types of inguinal hernia are distinguished, but they can only be precisely determined during surgery: The more common “indirect” and the less common “direct” inguinal hernia. Read more >
The indirect inguinal hernia follows the anatomically predetermined gaps in the groin, that is, it follows the spermatic cord, consisting of the vas deferens, testicular vessels, and muscular sheath, exits the abdomen through the inner (invisible) inguinal ring, follows the inguinal canal, and exits through the outer inguinal ring. Once it protrudes above the outer inguinal ring, it becomes visible and palpable.
The “direct” inguinal hernia bulges directly through a site of weak abdominal wall muscle behind the inguinal canal and then continues to the outer inguinal ring. The distinction is possible only during the surgery. It is important because a special surgical procedure is required for both types of inguinal hernias. The symptoms and examinations for both direct and indirect inguinal hernias are the same.
The inguinal hernia is primarily a male affliction and tends to affect young, athletic men with a slim build. Also affected are those who do very heavy physical work or are of an advanced age and have a prostate condition. The cause of the disease is due to a large pressure load in the abdominal cavity. Overweight, chronic constipation, pregnancy, heavy physical activity, chronic coughing in smokers, strong pressing in prostate enlargement as well as tumors of the colon are also among the co-factors.
An inguinal hernia, once it occurs, cannot regress. It gets bigger over time and usually causes increasing pain. The contents of the hernia sac may become trapped in the hernia gap and lead to disruption of the blood supply. Without treatment, the vessels close and the tissue may die. This necessitates high-risk, emergency surgery.
Symptoms of a hernia
“I can proudly say that I am a very athletic man. I jog frequently and do intense sports regularly. Recently, I have been experiencing increasing pulling pain in my right groin after running workouts. When I move or cough, the pain can intensify. A few days ago, while in the shower, I saw a small swelling the size of a walnut at the site of the pain, which was painful to the touch. The pain is now also moving to my scrotum and inner thigh. I am going to the doctor because I am now a little concerned after all.” Read more >
This story was told by one of our patients. It is quite typical. Patients usually first notice pulling pain in the groin area, and later see or notice a new onset of protrusion. Sometimes the protrusion forms without pain. It often occurs when coughing and laughing, pushing, exercising or carrying heavy loads. As it progresses, there may be increasing pain with everyday activities. Patients who have to carry heavy loads at work or do a lot of sport are particularly at risk. The swelling may be visible once at the beginning, later disappear. As a rule, however, it will become larger and larger until it is found to be really disturbing.
If the contents of the hernia (tip of the large mesh, intestine) are trapped in the hernia gap, there will be severe permanent pain at the site of the protrusion with radiation into the scrotum or pubic region. In addition to the swelling, there is redness and often a restriction of movement. The protrusion can be pushed back by the physician in some cases (without exception). Otherwise, emergency surgery cannot be avoided.
In principle, any abnormal protrusion in the groin area should be examined by a physician. In addition to hernias, enlarged lymph nodes or vascular changes may also be present. As long as there is no strangulated hernia, there is no reason for an immediate surgery. If the doctor diagnoses a hernia, it is usually possible to wait a few weeks before surgery.
It is very easy to overlook another type of soft tissue hernia called a femoral hernia. It is rare and is found on the inner thigh just below the groin. It passes through a gap that is open in the lower abdominal wall so that the great leg artery and the leg vein have a connection from the leg to the abdomen. A fracture of the thigh must always be presented to a doctor, as there is a high risk of entrapment.
Diagnosis for inguinal hernia
The focus of the physician’s questioning is primarily on the type, duration, and location of the pain. It is important whether the patient himself has seen a protrusion in the groin area or not. Further, it is important to know if there is chronic lung disease with a severe cough, problems with urination, or a tendency to constipation. Read more >
The workup is generally simple and consists of an inspection and palpation of the groin area by the physician. It is necessary to examine both sides while standing and lying down. The finding is often visible from afar when the hernia bulges into the scrotum. Additional tests are rarely required. In men, the inguinal canal is examined with the doctor’s index finger. Part of the scrotal skin is pushed against the inguinal canal with the fingertip. It can reach the outer inguinal ring through the skin.
Its size and shape, its diameter and the pain triggered by the examination are crucial. The protrusion of the hernia, the hernia sac, can often be palpated during this procedure. Sometimes the hernia occurs after straining or coughing, and often only its tip is palpated when it hits the tip of a finger while coughing. This is then referred to as a positive cough impact. Note whether both testicles are the same size and in the correct position in the scrotum. Further technical or imaging examinations are not normally required by experienced surgeons. In men over 40 years of age, a rectal examination should also be performed to palpate a possibly enlarged prostate.
In women, there is no external inguinal ring. A gap in the inner inguinal ring cannot be felt because it lies under the tight outer abdominal fascia (broad abdominal tendon). Below it, from the inner inguinal ring to the symphysis, runs the round maternal ligament. Therefore, if the findings are unclear, an ultrasound examination of the groin area is often performed in women. The ultrasound can show the different layers of the inguinal canal and often a gap with hernia content.
2. RUPTURE SURGERY
Rehabilitation of inguinal hernias
Need for surgery
In principle, all proven inguinal hernias should be surgically repaired today. Since soft tissue fractures cannot naturally regress, they become larger over time. If the diagnosis of an inguinal hernia is confirmed and the patient is in an operable condition, then there is no doubt that surgery is indicated. Depending on the symptoms, it can be determined when surgery must be performed. Only in patients who are in an inoperable state or refuse surgery should a hernia band be used. A hernia band is a very troublesome tool. It consists of a padded, elastic metal brace that is applied around the hips and a small ball-shaped leather bag that presses on the hernia gap. Since inguinal hernias can be operated on under general anesthesia, back anesthesia, or local anesthesia, which is convenient for the patient, the hernia band has only historical significance nowadays.
Surgical techniques
In modern surgery, depending on the findings, numerous different surgical procedures are used for inguinal hernias. There are open and minimally invasive methods as well as procedures with and without the insertion of synthetic mesh.
Open surgery of the hernia
The two most important open procedures are the Shouldice technique (named after the Canadian surgeon Earle Shouldice) also called transversoplasty, as well as the Lichtenstein technique, which requires the insertion of a mesh.
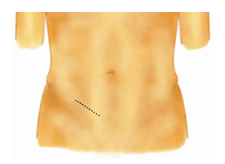
Through an oblique, approx. 6-8cm long, incision in the groin (Fig. 2), the skin and subcutaneous fat tissue are split.
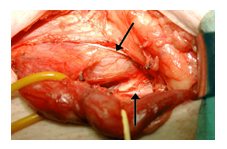
The outer inguinal ring is visited (Fig. 3), the fascia (tendon) is split and opened up to the inner inguinal ring.

Then the funicle (which includes testicular vessels, spermatic cord and muscular sheath) is dissected free up to the inner inguinal ring (Fig. 4) and looped with a yellow rubber band.
The inguinal ligament becomes visible (Fig. 5) and has a whitish sheen. In this example, a “soft” bar (no actual fracture formation) is visible.

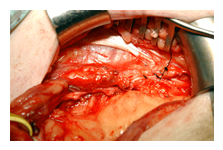
The funicle is treated separately. First, the cremasteric fibers (muscle sheath around the spermatic cord) are exposed. An indirect hernial sac is detached from the funicle and opened (Fig. 6). At its point of entry into the abdomen, it is ablated and closed with a suture.
A direct hernia sac is only pushed back into the abdominal cavity. The most important step is to split the posterior boundary wall of the inguinal canal, called the transversalis fascia (a taut, sheet-like band that lies in front of the peritoneum) (Fig. 7). The upper edge of the transversalis fascia is now displayed with the swab. Here it shimmers whitish and is held with tweezers. This fascial part is always well formed and gives the suture the necessary support for a firm and permanent anchorage. The inner inguinal ring must be left small in diameter, but still large enough so that the vascular supply to the testis is not compromised.


In women, the same procedure is followed, but the round mother’s ligament is included in the suture. The transversalis fascia is closed with a continuous suture starting at the periosteum of the pubis and extending to the inner inguinal ring (Fig. 8). The retracting suture then grasps the fibers of the inguinal ligament as well. After closure of the external fascia and subcutaneous fat, the skin is closed.
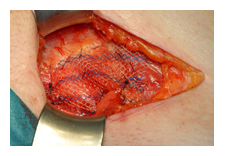
In the Lichtenstein procedure, a small, non-absorbable plastic mesh (made of polyethylene) is sewn in (Fig. 9). It is placed over the hernia gap and attached to the inguinal ligament and abdominal muscles in such a way that the gap can be closed without tension. A small opening must be left in the male for the passage of the spermatic cord. The mesh creates an areal scarring.
Minimally invasive surgery of the inguinal hernia

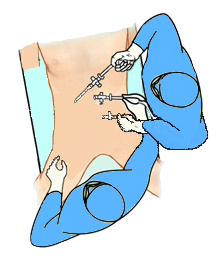
There are also different techniques for these operations. Common to all is the minimally invasive approach and the insertion of a plastic mesh. The procedure we use, TAPP, describes transabdominal preperitoneal mesh implantation. A small tube (trocar) is inserted into the abdomen through a small incision in the umbilical region. Subsequently, the abdominal cavity is filled with gas (carbon dioxide). Two more trocars are inserted (Fig. 10).
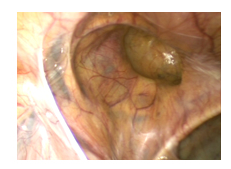
In minimally invasive surgery, the first step is laparoscopy, during which all organs accessible to the surgical method are examined. Both groins are then inspected (Fig. 11) and a decision is made as to whether the fitting should be performed on one or both sides.
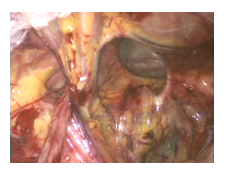
In preparation for mesh insertion, the peritoneum is opened (Fig. 12) and the hernial sac is completely dissected free. In doing so, the spermatic cord and its accompanying vessels are spared. Minor bleeding is stopped immediately.
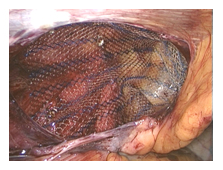
Subsequently, an approx. 10x15cm plastic net is inserted and fixed in place. Fixation is performed using tissue adhesive or dissolving staples (Fig. 13).
Finally, the opened peritoneum is closed over the implanted mesh (Fig. 14). The gas is drained and the three small skin incisions are sutured.

Is open or minimally invasive surgery right for me?
This question cannot be answered in general terms. Surgeons today have a wide range of procedures available for inguinal hernia surgery. According to the studies available to date, it is not possible to declare conclusively which of the methods is the best. What is certain, however, is that today the necessary procedure can be used depending on the findings and the patient. In addition, it is necessary to consider with which method a surgeon has the greatest experience. Read more >
It is considered certain that in the event of a relapse (recurrence) after open surgery, a method with mesh insertion promises more success, and a minimally invasive method should also be used rather for bilateral surgeries. In addition, significantly less pain is described here, and mobilization is correspondingly faster. We will be happy to explain in detail the advantages and disadvantages of the surgical procedure that is suitable for your case.
For open surgery, with or without mesh, either local, spinal or general anesthesia is used. The minimally invasive procedures can be operated only under general anesthesia.
What happens after the treatment?
The patients can already get up on the day of the operation and eat something light. Appropriate medications and decongestants are administered for pain management. The stay in the hospital is very short. Some patients have the surgery performed on an outpatient basis. On the day of the surgery, in rare cases, due to the gas supply in the tissue, there may be swelling of the scrotum or labia, which persists for a few days and completely disappears. Read more >
Complications after these procedures are rare. Wound infections and bleeding can occur, but are easily treated. Very rarely, more severe problems occur: vas deferens, testicular vessels, or nerves may be injured in the groin area or irritated by natural scarring. If nerves in the surgical area have been crushed or severed, this can lead to temporary sensory disturbances in the area of the thigh or groin. If the testicular vessels are injured, this can lead to testicular shrinkage.
Temporary sensory disturbances in the area of the wound and the skin on the thigh may also occur. Infection of the mesh or its displacement with ingrowth against the vas deferens or against the bladder are extremely rare. The risk of developing a new fracture is generally around one to four percent for all procedures.
What must be paid attention to in the future everyday life?
Carrying loads of more than three kilograms should be avoided for six weeks after the operations. The incapacity to work therefore also varies between a few days and a few weeks depending on the occupation. After two months, the healing is complete and there are no further restrictions.
Historical
Soft tissue fractures were already known in ancient Egypt. An ancient papyrus described soft tissue hernias in the groin, which were common at the time, as early as about 3,500 years ago. Because of the protrusion, which becomes larger over time, the ancient Greeks called soft tissue hernias “hernios,” which means “bud.” In technical jargon, it is therefore still referred to as a hernia. Read more >
In ancient times, soft tissue fractures could only be treated with compressive pressure bandages. In the Middle Ages, hernias were cut open by so-called hernia cutters at the fairs. The hernia sac was removed during this procedure and the intestinal contents were pushed back into the abdominal cavity without any anesthesia or without sterile work. The results in these unfortunate patients were disastrous. Most died during the surgery or within a few days due to peritonitis. In the few patients who survived surgery, the hernia recurred because the hernial orifice in the groin was not closed.
It was not until 1890 that Edoardo Bassini (1844-1924), at the Royal University of Padua, introduced a surgical technique in which the posterior wall of the inguinal canal was tightly sutured. Bassini was a full professor of pathological anatomy and surgery at the University Hospital of Padua from 1883 and had spent years studying inguinal hernias, which were untreatable at the time. In 1890 he published 262 surgeries using his method in the “Archive for Clinical Surgery”. The Bassini surgery was already then a modern and safe method, which was successfully performed for almost 100 years. This technique was considered the standard procedure worldwide. Only in recent decades have refinements been made to this technique and new processes developed.
A very successful variant of the Bassini procedure has been successfully introduced at the Shouldice Clinic in Canada [1]. This was followed by completely new, open surgical procedures in which plastic meshes were sewn in front of the hernia gap according to the surgeon Lichtenstein’s method. In the very new minimally invasive methods, these meshes are placed over the abdominal cavity, or behind the trunk muscles and in front of the abdomen. Thus, a variety of surgical procedures, both open and minimally invasive, are available today for the treatment of inguinal hernia.
