Extra Information
Warning
The diseases described on the following pages contain images and film material taken during operations. Decide for yourself if you want to see these images. Please also note our imprint and the legal information. The Baermed practice assumes no liability. Do you really want to see the page!
Appendix
Topics
1. Appendicitis
Symptoms and surgery for appendicitis
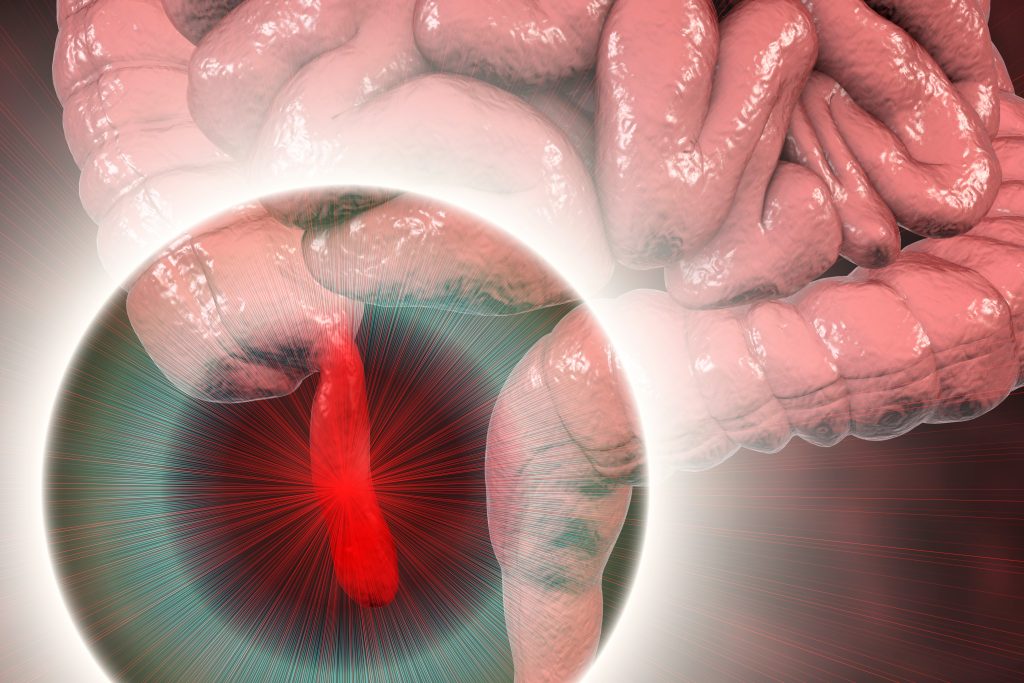
Appendicitis is the inflammation of the appendix of the appendix. It is also called appendicitis. The appendix is located in the right lower abdomen and may have a different location.
Appendicitis can have different degrees of severity and is divided into three conditions accordingly:
- a) Appendicitis phlegmonosa = inflamed
- b) Appendicitis gangrenosa = disintegrating
- c) Appendicitis perforata = ruptured
Where is the appendix located?
The appendix or vermiform appendix is a ten to twelve centimeter long appendage at the top of the colon and is about one centimeter thick. It is referred to by the term “appendix” because it ends without an exit. The name “appendix” comes from its worm-like shape. It is called in technical language and in Latin “appendix vermiformis”, in German the appendix. The appendix is located a little differently in each person, for example, in front of or behind the colon. (Fig. 1) It may be turned up against the liver or fully extended into the lesser pelvis. In the latter place, it can also have very close positions to sex-specific organs in women.

How does the appendix work?
To this day, it is still not completely clear what the significance of the vermiform appendix is. It is believed to play a role in the body’s defense function. However, it is not essential for life.
The acute inflammation as the most common disease of the appendix
During detection (so-called diagnosis), the word “acute inflammation” often comes up. In acute inflammation, the tissue is attacked by pathogens that cause a defensive reaction. Specialized cells of the body fight the invaded pathogens and try to kill them. This reaction is called inflammation. If it starts suddenly, it is called “acute”. See Figure 2.
In acute appendicitis, these defensive reactions take place in the wall of the appendix. Feces and pus collect inside the appendix. If the entire wall is riddled with foci of pus, the wall may rupture and the contents of the appendix may leak into the free abdominal cavity. This “burst appendix” is quite dangerous situation, because the inflammation can spread to the peritoneum and after after a while they can poison the whole body. For this reason, in the more than one hundred years of history of appendicitis, physicians learned that life-saving surgery must be performed as early as possible for such a condition.
Read more >
At the same time, appendicitis is common. It affects people of all ages and both sexes. Young patients and also children are frequently affected by acute appendicitis. Appendicitis can be dangerous for elderly patients or for patients who have a weak immune system. It can occur in old age and after previous serious illness. Anti-inflammatory drugs or those needed to weaken the body’s defenses after organ transplants can also lead to immune deficiency.
The cause of acute appendicitis is bacterial colonization of the appendix, caused, for example, by fecal or fecal stone buildup in the organ without exit. However, ingested cherry pits with water are unlikely to play a role. Although the doctors do not know exactly about the ultimate causes of the disease, they are clear about how it can be cured: with surgery. And again, let it be said: the appendix is not a vital organ.
Symptoms of appendicitis appendix?
“Actually, I should have done some important work at the store in the morning. However, when I got up, I felt very unwell, and I could not eat breakfast. Before leaving, a strong nausea suddenly appeared. I stayed at home. I had to vomit, and somehow diffuse pain appeared around the navel area. I suddenly had a fever over 38 degrees, and the pain was now felt in my right lower abdomen. I could point my finger to the spot in my right lower abdomen where it hurt the most.”
Read more >
Patients cannot always give such precise information about their disease. But today, even a few clues are enough to raise the doctor’s suspicion of appendicitis. An important, almost characteristic pain point is the so-called McBurney point. It is located in the middle of a line between the anterior right pelvic bone and the navel. If the disease spreads because surgery is not performed early, the appendix may rupture.
In the process, the pain can almost disappear completely in the short term. They return when the inflammation spreads to the peritoneum and spreads throughout the lower abdomen. The pain follows the progression of the inflammation and may be felt throughout the lower abdomen, including on the left side. Especially when walking and standing up, they can become very strong. The patient often obtains pain relief by lying down and tightening the legs in the supine position.
Diagnosis and clarification of appendicitis
At the beginning of each examination, the doctor asks the patient questions. In the case of the appendix, these are questions about the type, duration, and occurrence of pain, about urination, and about bowel movements. In women, additional gynecological questions are asked, for example, about menstruation, bleeding and discharge. Further, the temperature is measured both in the anus and under the armpit. As a whole, the four series of examinations listed below usually allow the physician to correctly diagnose appendicitis:
Read more >
Examination of the abdomen with hands
The physician looks for the typical pain points (McBurney point) and for an involuntary defensive tension of the muscles when the abdominal wall is pressed in (défense) and the pain when the pressing-in hand is suddenly released (release pain). He also looks for pain when tapping on the abdomen (tapping pain) and for shaking pain, in which he shakes the patient.
Rectal examination
Examination of the rectum is best performed in the supine position with the physician’s index finger. Although this examination is somewhat uncomfortable, it provides crucial clues to the correct diagnosis. The physician inserts the index finger, covered with a plastic glove and fingerstall, into the anus over the sphincter. Of course, he uses a lubricating cream so as not to cause pain. In men, the prostate is examined at the same time; in women, the cervix and any pain sensitivity of the uterus are examined. Such an examination is absolutely necessary. A physician can be held legally liable for failing to perform a rectal exam when appendicitis is suspected.
Laboratory tests
The blood drawn from the patient provides evidence of inflammation. Further examination of the urine excludes infections of the kidneys and urinary tract.
Imaging procedures: Ultrasound imaging is used to visualize the appendix, but the entire abdomen with the draining urinary tract and with the bladder, kidneys, gallbladder and liver is also examined. In women, the ovaries and fallopian tubes additionally appear. Sometimes an ultrasound examination through the vagina is necessary to rule out gynecological disease. If the findings are unclear, X-rays are often taken in the supine and standing position, or a computer tomography with contrast medium is performed.
Acute appendicitis
Recognizing acute appendicitis is often very difficult. Although the disease is very common, it is often misrecognized. Doctors sometimes speak somewhat casually of the “monkey in the belly” because appendicitis can “mimic” or fake so many other diseases. Therefore, the listed examinations are important. Together they form a whole that usually allows the correct diagnosis of appendicitis. In rare borderline cases, the experience of the treating surgeon is still important. He also has laparoscopy at his disposal as a further imaging procedure with which he can look through a small opening in the abdomen (see “Laparoscopic surgery” below).
2. Treatment of acute appendicitis
At the beginning of acute appendicitis, the disease can be difficult to diagnose. Therefore, antibiotics and painkillers are often administered on a trial basis. However, they cannot cure appendicitis. If in the later course of the disease and through often repeated examinations it becomes clear that it is appendicitis, surgery must be performed. Today, there are two modes of operation. Both must be performed under general anesthesia.
The open surgery
Through an incision about six centimeters long in the right lower abdomen, the skin, subcutaneous tissue, muscle skin and abdominal wall muscles are cut. The peritoneum is opened and the view is kept clear with small hooks. The colon is manually pulled into the wound, and the tip of the appendix is grasped. The small suspensory ligament of the appendix is cut between two sutures. A so-called tobacco pouch suture is placed on the colon around the base of the appendix. Subsequently, the appendix is tied around and removed. The small stump of the appendix is subsequently placed under this tobacco pouch suture and the suture is fixed over it. The abdominal wall is then closed again in layers. If a collection of pus was previously found around the appendix, this pus cavity is drained with a small plastic tube.
The laparoscopic surgery
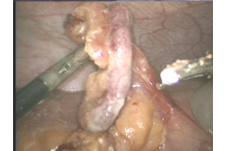
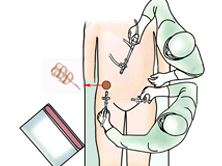
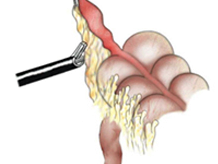
Today, the so-called “keyhole surgery” is increasingly used for appendectomy. For this purpose, the abdominal cavity is first filled with warmed gas through a small hollow needle at the navel. A skin incision of one centimeter in length is made at the navel. A sterile video camera is inserted into the abdomen through this opening. The surgeon can see into the abdomen via this camera on a screen. Working instruments such as small scissors and clamps are inserted through two, five-millimeter incisions each in the left and right lower abdomen. (Fig. 3)

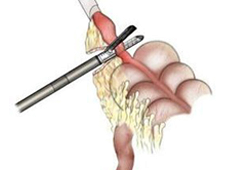
They can be used to grasp the appendix and cut its suspensory ligament with a special device (e.g., ultrasound dissector). (Fig. 4)
The appendix is cut off at its base just in front of the wall of the colon using a special stapling device. (Fig. 5)
The diseased organ is removed through the small incisions. (Fig. 6) The small skin incisions are sutured. In patients with certain previous operations and adhesions, the appendix can occasionally be removed only with open surgery.
What happens after the treatment?
“When I woke up from the anesthesia, I still had slight pain in my lower abdomen. But I was surprised how quickly I felt better again. I was allowed to drink tea and water the same day and had to stand up briefly. By the second day, I was already eating light again, and I was fine.”
In both open and laparoscopic surgery, the patient can usually get out of bed and drink a little on the same day. On the second day, he is allowed to eat again. In the case of a “burst” appendix, an antibiotic may need to be taken for a few days. The small tubes of any drainage can be pulled out of the wound four to six days after surgery. As with any surgery, complications cannot be ruled out with appendectomy. Fortunately, however, these are relatively rare in this procedure. They are well known to doctors and can be treated well. Harmless wound infections are most common, and abdominal complications rarely occur.
What must be paid attention to in the future everyday life?
The disease is definitely cured after the operation. Those who have undergone surgery can continue to live normally. There is a very small risk that adhesions may form as a result of surgery years or decades later, leading to bowel obstruction. Such a one would have to be operated in any case.
Historical
The disease of appendicitis has been known since the Middle Ages. Already in the 16th century it was found and described during corpse openings. In the 18th century, the disease was first diagnosed in a living patient. James Parkinson described peritonitis in 1812, which at that time followed appendicitis. Although the disease was recognized as dangerous, treatment was carried out with traditional methods such as bloodletting, leeches and enemas. It was not until 1886 that the American anatomist Reginald Heber Fitz in Boston designated inflammation of the appendix as the cause of the disease. He created the word appendicitis (“appendicitis”) and demanded – most radically for ears of that time – the complete surgical removal of the diseased organ. Read more >
Who had the courage to perform the first appendectomy is not entirely clear to this day. Robert Lawson Tait in 1880 in England, Rudolf Ulrich Krönlein in 1886 in Germany, and also George Thomas Morton in 1887 in the USA, all performed operations on the appendix. The first interventions were performed late in the course of the disease and after the acute inflammatory signs had subsided. Surgeons drained only the pus or removed part of the appendix. It was not until the Chicago surgeon John Benjamin Murphy that the now common and early surgical procedure was introduced. He requested that the appendix be removed entirely before the inflammation allowed pus to pass through the wall of the appendix into the abdominal cavity. There were few who believed him at the time. The belief in treatment with drugs was still too widespread and the technology and knowledge of the few courageous surgeons in the USA as well as in Europe were not mature enough. European physicians smiled at the “wild Americans” anyway. And surgeons were troublesome competition for them.
The breakthrough of appendectomy came on June 24, 1902, when the English Prince of Wales fell ill with appendicitis shortly before his ceremonial coronation as King Edward VII – a political and social catastrophe for the then world power Great Britain. After dramatic symptoms and futile medical treatment by the court physician, Frederick Treves undertook the saving operation on the king in the presence of Joseph Lister, the aged discoverer of antisepsis, which is indispensable for all operations. He drained the pus, and King Edward VII recovered. In gratitude for saving his life, Treves was given the (hereditary) title of baron.
Today, the operation of the appendix (appendectomy), which has now been practiced for over 100 years, is undertaken as early as possible after the disease is detected. Appendicitis is the most common gastrointestinal condition and the abdominal surgery in which physicians have the most experience.
