Extra Information
Warning
The diseases described on the following pages contain images and film material taken during operations. Decide for yourself if you want to see these images. Please also note our imprint and the legal information. The Baermed practice assumes no liability. Do you really want to see the page!
STRONG OVERWEIGHT
Topics
1. obesity (morbid overweight)
Chronic nutritional and metabolic disease
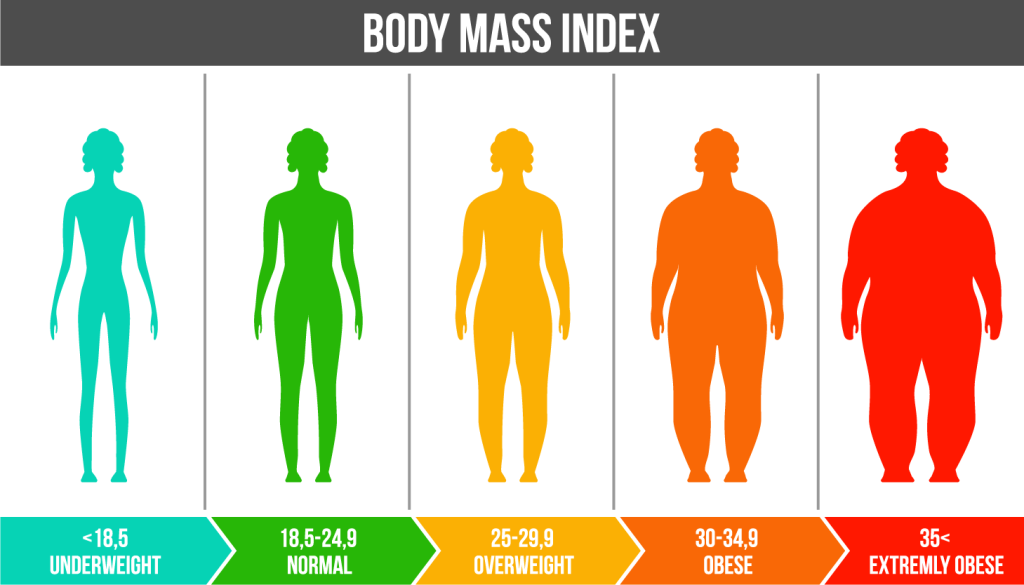
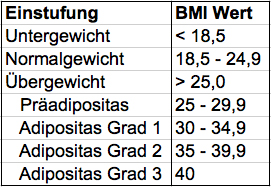
In obesity, i.e. severe overweight, an excessive amount of fatty tissue accumulates in the body. A person is considered overweight (obese) if his or her body mass index (BMI) is over 30. The body mass index is calculated by dividing the body weight in kilograms by the body height in meters squared.

How does morbid obesity develop?
Obesity, which is becoming increasingly widespread in the western world, is essentially the result of a long-term positive energy balance. This occurs when the amount of energy consumed daily with food is greater than the body’s energy expenditure. Well over 90% of obesity cases can be explained in this way. Read more >
In addition to the wrong eating behavior (high-fat meals, irregular intake of food), the lack of exercise is crucial for weight gain. Numerous social factors and factors that characterize our culture support the rapid spread of morbid obesity, which the World Health Organization (WHO) believes is an epidemic. These include the increasingly passive use of leisure time (computer, TV), the advertising strategies used by the food industry for high-energy foods and sweets, the growing prevalence of fast food and convenience foods, the permanent oversupply of goods, but also food as a substitute for a lack of integration and attention as a result of increasing professional involvement and competition as well as social tensions. In a few cases, metabolic diseases or the use of certain medications can cause or promote obesity.
The role of genetic factors has been intensively researched for years and cannot be definitively answered at this time.
Why is obesity so dangerous?
Obesity can cause or exacerbate numerous secondary diseases with considerable risks for the body. The most common are high blood pressure, increases in blood lipids and cholesterol, diabetes mellitus, various joint disorders, sleep apnea syndrome, vein disorders, but also mental balance disorders (depression) and sexual disorders. Particularly dangerous is the combination with several secondary diseases as is the case with the metabolic syndrome (obesity and hypertension, diabetes mellitus, hypercholesterinaemia). As a result of the diseases mentioned, the risk of a heart attack and stroke increases significantly compared to the population of normal weight Read more >
If the described changes persist for a longer period of time, numerous irreversible changes in the organism occur that require permanent treatment and significantly reduce both the quality of life and the life expectancy of those affected. Due to the stigmatization of overweight (beauty ideal) practiced by the environment, patients often become lonely, which leads to social disintegration and, in addition to personal consequences, also has serious social consequences.
The connection between morbid obesity and some malignant tumor diseases (breast cancer, uterine cancer, colon cancer, prostate cancer) is regarded as established.
2. Treatment options
Prevention and treatment
Prevention
The prevention and treatment of obesity pose an extraordinary challenge to all involved. At the present time, it must be assumed that more than 2 million Swiss people are overweight, and the number is constantly increasing. Of particular concern is the increase in childhood obesity. This is countered by numerous conservative and surgical treatment strategies. The basis of any therapy is the change of lifestyle habits as well as the change of dietary behavior. Despite countless diet programs and fasting “cures”, only a very small proportion of those affected can permanently maintain the weight reduction achieved.
The vast majority of overweight people gain weight again after the end of food restriction and often reach a higher weight than the initial weight. The cause is the lowered energy metabolism during the diet, so that an immediate increase in weight is recorded when “normal” food is consumed later. In addition, even with a strict, long-term diet, a weight reduction of more than 5kg/year can rarely be achieved. Read more >
Increasing physical activity is another building block for reducing excess weight, but here, too, long-term success can only be assumed if habits are fundamentally and permanently changed. According to available experience and studies, the drug therapy for (rapid) weight loss proclaimed in particular in the media is accompanied in almost all cases by side effects, some of which are severe, and is rarely as successful as promised. It is not an alternative to the above strategies.
The most important and only promising conservative treatment option is the consistent prevention of obesity, starting in childhood. Ultimately, surgical intervention is the last resort for morbid obesity. This is now also recognized by leading nutritionists.
3. Surgical techniques
Gastric bypass and gastric banding surgery for obesity
Body mass index and the three obesity severity levels
The WHO classifies weight according to the so-called body mass index (BMI). This describes the body weight in relation to the body size and is defined in kg/m². Overweight is defined as a BMI of >25kg/m².
Obesity, which is divided into three degrees of severity, begins at a BMI >30kg/m².
In principle, the need for surgery is determined on the basis of numerous parameters, whereby this must be done taking into account the legal requirements based on existing medical knowledge.
These include a consultation with the medical examiner, a BMI of at least 40kg/m², an age limit (not >60years), at least two years of unsuccessful conservative therapy for obesity, the presence of at least one concomitant disease (hypertension, diabetes mellitus, hypercholesterinaemia, sleep apnea syndrome, heart disease, etc.) and the condition that the care before, during and after surgery is provided by a team of physicians familiar with the clinical picture.
Surgical therapy can also be performed in certain cases with a BMI >35 kg/m².
Obesity severity levels 1 to 3
How much weight can I lose through the surgery?
Depending on the type of surgery, the obese person loses between 40-70% of their excess weight (called excess weight loss), with a slight regain of weight usually occurring after a few years. The weight reduction is greatest in the first two years and slows down in the following.
What clarification must be made before the operation?
The clarification necessary for the intervention is carried out by a medical professional experienced in the treatment of obesity. For this purpose, several consultations and close cooperation with the family doctor are usually necessary. In addition to the weight history and eating habits, the secondary diseases, the social environment (family, work), a psychological assessment and the patient’s willingness to cooperate are clarified as part of the preliminary examinations. In addition, the cost approval of the health insurance must be available. Read more >
The presence of an interdisciplinary team (metabolic physician, bariatric surgeon, anesthesiologist, intensive care physician, psychologist) is crucial in order to provide the patient with all-round competent care. This basic prerequisite is given at all times by the very close cooperation with the colleagues of the metabolic center specialized in the treatment of obesity, the highly competent team of anesthesia and intensive care medicine and the cooperation with the psychologists. All patients are discussed together with all specialists at an interdisciplinary obesity board prior to surgery. At the time of hospital admission, the diagnostics are supplemented and completed by some examinations necessary for the operation (laboratory, ECG, X-ray of the lungs, pulmonary function test).
Two different surgical techniques
For the surgical treatment of obesity, we have a choice of various procedures, which are all performed using minimally invasive techniques, provided that there are no contraindications (exclusion criteria). This makes it possible to achieve a significant reduction in general and specific risks. All techniques are based on the mechanisms of restriction (limiting food intake by reducing the gastric reservoir), malabsorption (limiting food intake by later combining food and digestive juices) or their combination. In addition to the mechanisms of action described above, hormonal effects play an important role, since the operation reduces the feeling of hunger.
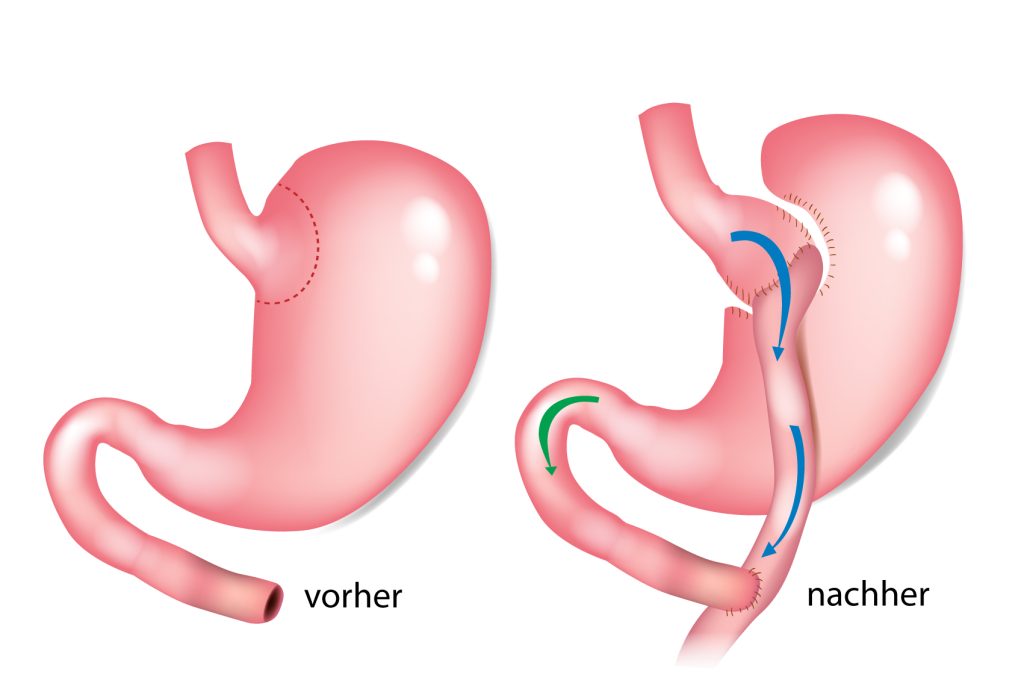
Gastric Bypass
Gastric bypass is based on the combination of food restriction and malabsorption. For this purpose, a small portion of the stomach is separated from the rest of the stomach and then reunited with a loop of small intestine. In this way, in addition to reducing the size of the stomach, it is possible to achieve a later coming together of ingested food/drinks and the bile and pancreatic juices necessary for digestion. As a result of the newly created passage, insulin production is influenced so that within 3 months up to 80% of type II diabetics can stop their drug or insulin therapy. The weight loss to be recorded is usually 70% of the excess weight in the first year after surgery. Read more >
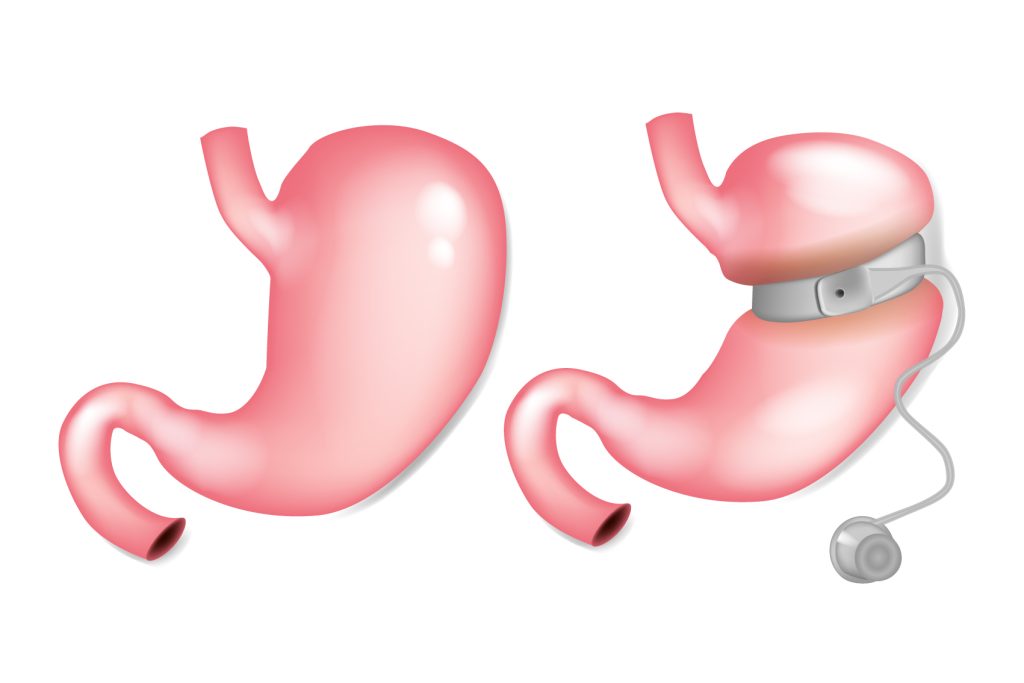
The (controllable) gastric band causes a pure restriction. It is passed around the upper part of the stomach, also using a minimally invasive technique, creating a small “pre” stomach. The width of the gastric band can be controlled by a so-called port system inserted under the skin. By implanting a gastric band, the size of the food portions is greatly limited by mechanical means; in addition, a rapid feeling of satiety is achieved. The average weight loss is about 50% of the excess weight and good compliance (cooperation) of the patient is essential.
Tubular gastric banding (gastric band)
Another restrictive procedure is tube stomach formation. It is also based on the principle of food restriction, but as a result of the resulting reduced gastric acid production and hormonal effects, the feeling of hunger is also reduced. The surgery involves the complete removal of a portion of the stomach, leaving a narrow gastric tube in place. This intervention is also performed laparoscopically. Read more >
The operation can usually achieve a weight loss of 50-70% of excess weight in 2 years, assured long-term results on the method are still pending. In some cases, after gastric banding implanted in the past, it is necessary to remove the gastric band and apply gastric bypass in the same operation, especially in case of lack of weight reduction or renewed stronger weight gain.
All interventions require both a surgeon experienced in laparoscopic and especially in bariatric surgery as well as appropriate surgical-technical requirements.
Which surgery is right for me?
This question can only be answered after a thorough evaluation of the medical history, the diagnostics and the evaluation of the findings as well as the perioperative risks in a joint discussion. The patient is shown the mode of action of the individual methods, the risks, advantages and disadvantages of the procedures, and any questions that arise are answered. It is important to have an assessment by a team of physicians and psychologists experienced in obesity treatment.
What happens after the surgery?
After the intervention, patients are transferred to the intensive care unit, where they usually stay until the next day. On the day of the surgery, the surgeon makes a visit during which important parameters are assessed and an initial discussion is held on the course of the intervention. On the first day after the operation, patients are transferred to the normal ward, and an X-ray examination is also performed to check the results of the surgery. If the findings are unremarkable, patients can begin drinking. In parallel, with the help of physiotherapy begins mobilization Read more >
n the 3rd day after surgery, another X-ray control is performed. This is followed by the gradual build-up of the diet. Any drains inserted during surgery are removed. The patient is visited twice a day by the surgeon to discuss any questions or problems. At the same time, the colleagues of the Metabolic Center and the Nutritional Counseling Center are closely involved in the care of the patient. Once the food buildup is complete, patients can be discharged, usually on the 7. until 8th day after surgery can be discharged home. After one week, another outpatient check-up is performed in our practice. Here, too, questions can be clarified and initial impressions regarding the surgical result can be discussed.
What needs to be considered for the future?
All bariatric surgical procedures require long-term, skilled follow-up care. The aim is to avoid complications and to monitor progress and ensure long-term success. In addition to the clinical examination, regular weight monitoring, it includes the collection of laboratory parameters and current eating habits. As a result of the operation, substitution (replacement) of some vital substances (iron,vitamins, calcium) is necessary. Due to the massive weight loss, in numerous cases it is necessary and desirable to consult a plastic surgeon in the course.
